Month: April 2020
Gut microbiome linked to efficacy of PD-1-inhibitor therapy for solid cancers
In patients with solid cancers, the concentration of fecal short-chain fatty acids (SCFA) may be a biomarker of the efficacy of the programmed cell death 1 (PD-1) checkpoint inhibitors nivolumab and pembrolizumab, according to researchers in Japan.
Immune-checkpoint inhibitors have been remarkably effective across multiple cancer types, note Dr. Motoo Nomura of Kyoto University and colleagues in JAMA Network Open. However, for solid cancers the response rate to PD-1 inhibitors has been relatively low, they add.
Thus, a biomarker of efficacy “is critically needed for clinical decision-making,” they say, and the gut microbiome profile could be one such factor.
To investigate, the researchers prospectively studied 52 cancer patients with a median age of 67 years who were scheduled to be treated with nivolumab or pembrolizumab. Concentrations of SCFAs in fecal and plasma samples were determined before PD-1 inhibitor administration.
The overall response rate was 28.8% and the median follow-up of survivors was for two years. There were no significant differences between responders and nonresponders in patient characteristics,
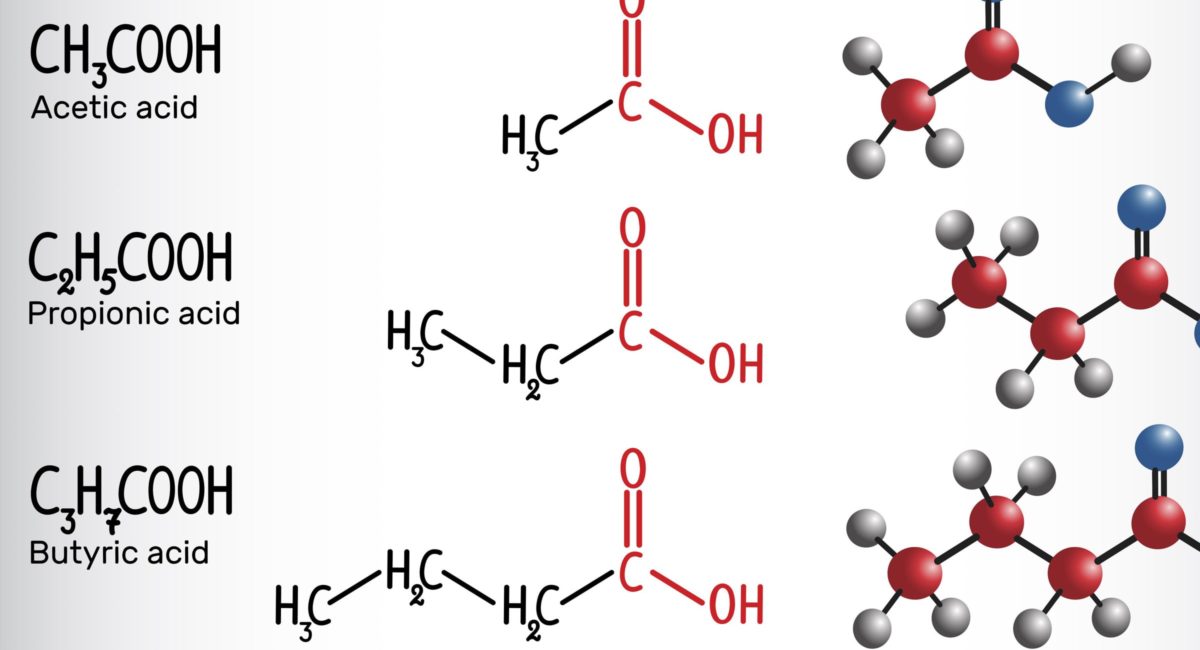
However, concentrations of fecal and plasma SCFAs were higher in the responder than nonresponder group, and high concentrations of some SCFAs were significantly associated with longer progression-free survival. These included fecal acetic acid (hazard ratio, 0.29), propionic acid (HR, 0.08) and butyric acid (HR, 0.31). This was also the case for plasma isovaleric acid (HR, 0.38).
The results, the researchers say, “showed that high frequencies of intake of several sources of dietary fiber, such as green vegetables, cabbage, and mushrooms, were associated with high concentrations of fecal SCFAs.”
There was no significant association between green vegetable or cabbage intake and progression-free survival. However, Dr. Nomura told Reuters Health by email, “A high frequency of mushroom intake during the one year preceding the onset of their current cancer was significantly associated with longer progression-free survival (HR, 0.40) in patients with solid cancer tumors treated with programmed cell death-1 inhibitors.”
However, he and his colleagues stress that the dietary information used in their study was collected before it started.
The researchers call for further studies but suggest that SCFAs may be the link between the gut microbiota and PD-1-inhibitor efficacy.
“Because fecal examinations are completely noninvasive, they may be applicable for routine monitoring of patients,” they say.
Continue Reading


